
Significant advances were made in treating tumors of the brain, lung, and pancreas. Efforts to improve surgical quality included accrediting cancer programs, certifying surgeons, and setting minimum standards for surgical residencies.
1931
Neurosurgery Society Founded

1931
Neurosurgery Society Founded
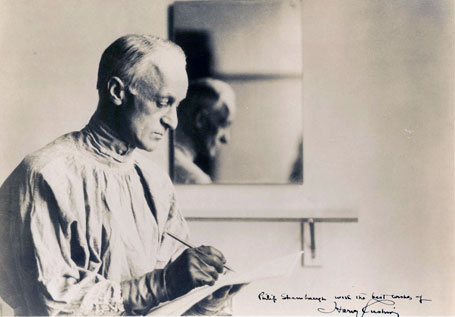




The Harvey Cushing Society, the precursor to the American Association of Neurological Surgeons, was founded in the name of the "father of modern neurosurgery," Harvey W. Cushing, MD, FACS.44 "Cushing became the first surgeon in history who could open what he referred to as 'the closed box' of the skull of living patients with a reasonable certainty that his operations would do more good than harm," the medical historian Michael Bliss wrote in Harvey Cushing: A Life in Surgery.45,46 Dr. Cushing performed the first brain surgery in the U.S. in 1901 and completed his 2,000th tumor operation in 1931. He also discovered that pituitary tumors could lead to vast changes in the body; "Cushing's disease" and "Cushing's syndrome"—two illnesses linked to hormones gone awry—are named for his discoveries.47
Dr. Cushing's dedication to evidence-based medicine is nowhere more apparent than in the Cushing Brain Tumor registry, an immense archival collection of more than 2,200 case studies that includes human whole brain specimens, tumor specimens, microscopic slides, notes, journal excerpts, and more than 15,000 photographic negatives dating from the late 1800s to 1936. The collection had been moved a number of times before being sequestered in a sub-basement of a Yale University dormitory in 1979. By that time, few paid much attention to it except for intrepid medical students who, as part of a "rite of passage," snuck through the dark, dank passageways to visit the "brain room."48 In 2010, the collection finally got its due when it was put on permanent display at the new Cushing Center at Yale University's medical library.
Citations
1931
College Accredits First Hospital Cancer Programs
1931
College Accredits First Hospital Cancer Programs

In 1931, the College initiated surveys of cancer programs in hospitals49 and accredited the first three hospital cancer programs. The accreditation was based on standards for evaluation of cancer clinics and registries published a year earlier by the College's Committee on the Treatment of Malignant Disease (established in 1922), the precursor to the Commission on Cancer (CoC).50 In 1933, the College published its first list of approved institutional cancer programs.51 Since then, the standards for cancer programs have been revised and expanded to reflect the comprehensive scope of cancer programs, the multi-disciplinary nature of cancer care and the continuous changes in the health care environment. The accreditation program was designed to ensure that the structures and processes necessary for quality cancer care are in place at the facilities providing care to patients with cancer. Today more than 1,500 hospitals in the United States and Puerto Rico are CoC accredited, representing only 30 percent of all institutions but more than 70 percent of all new cancer cases diagnosed annually.
Citations
1933
Thoracic Surgery Techniques Pioneered

1933
Thoracic Surgery Techniques Pioneered
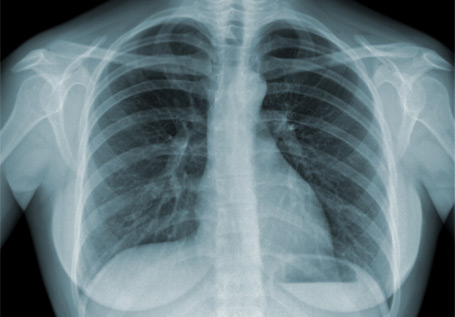


At a time when the mortality rates from lobectomy (excision of the lobe of the lung) were about 50 percent due to unrefined techniques and septic complications, Edward D. Churchill, MD, FACS, was able to show how to safely and selectively remove diseased parts of the lung. For instance, in November 1933, he performed the first single-stage resection of the right lung for adenocarcinoma.52 Dr. Churchill would go on to develop surgical techniques to treat bronchiectasis, pulmonary tuberculosis, and lung cancer.
Citations

1935
The American Debut of the "Whipple Procedure"
1935
The American Debut of the "Whipple Procedure"

Allen O. Whipple, MD, FACS, a Columbia University surgeon, was the first American to perform a complex operation for treating pancreatic cancer, now known as the "Whipple Procedure." The procedure, which is technically called a "pancreaticoduodenectomy," involves removing the head of the pancreas (called the duodenum), parts of the bile duct, and the gallbladder, and sometimes part of the intestine, after which the remaining intestine, bile duct and pancreas are reconnected.53 Dr. Whipple once said of the procedure named for him that "the considerable risk [of operative mortality] of 30–35 percent is justified if they [the patients] can be made comfortable for a year or two."54 The Whipple Procedure remains one of the few effective treatments against pancreatic cancer, which is one of the deadliest and toughest cancers to treat.
Citations
1937
First Blood Bank Opens in Chicago

1937
First Blood Bank Opens in Chicago

Bernard Fantus, MD, introduced the term "blood bank" to describe a new blood donation, collection, and preservation facility at Cook County Hospital in Chicago, where he served as director of therapeutics. Later that year, Dr. Fantus published in precise detail the principles of organizing a blood bank in the Journal of the American Medical Association. This article gave hospitals worldwide a master plan of their own to follow—and likely saved thousands of lives, given the advent of World War II. Within a few years, hospital and community blood banks were established across the United States and Europe,55 and the idea revolutionized surgery and transfusion therapy.
Citations

1937
American Board of Surgery Founded to Certify Surgeons
1937
American Board of Surgery Founded to Certify Surgeons

Arguing that the College was not doing enough to establish "proper standards of qualification of those permitted to practice surgery," Evarts A. Graham, MD, FACS, proposed the development of an independent certifying board.56 Within two years, Dr. Graham's dream was realized: In 1937, the American Board of Surgery, an independent, nonprofit organization, was created to establish a certification process and national certifying body for surgeons practicing in the U.S. The board, whose mission was to protect the public and improve the specialty, was created by a committee assembled by the American Surgical Association with representatives from the American College of Surgeons, American Medical Association, and the Western, Southern, New England, and Pacific Coast Surgical Associations.57 The leaders of these organizations felt surgery had matured into a full-time specialty and recognized the need to differentiate well-trained surgeons from doctors in general practice.
Citations
1937
Minimum Standards Set for Surgical Residencies

1937
Minimum Standards Set for Surgical Residencies

Minimum standards were set for surgical residencies and field surveys of programs were initiated. Later, the first Residency Review Committee (RRC), the RRC for Surgery, was established in 1950 as a collaboration of the College, the American Medical Association, and the American Board of Surgery.58 Similar collaborative RRCs were subsequently established for colon and rectal surgery, neurological surgery, otolaryngology, plastic surgery, thoracic surgery, and urology. These committees have set high standards of quality for graduate surgical education that are used in evaluation and accreditation of surgical residency programs in the U.S.59 Currently, there are RRCs for 27 of the specialties in medicine.60
Citations

1939
Study Published Linking Tobacco Use to Cancer
1939
Study Published Linking Tobacco Use to Cancer



In 1919, lung cancer was such a rare disease that when Alton Ochsner, MD, FACS, was a junior in medical school at Washington University's Barnes Hospital, his entire class was asked to witness the autopsy of a man who had died from it. His professor, George Dock, MD, believed that no one in the class would ever again see another such case. In fact, it wasn't until 17 years later that Dr. Ochsner saw his next case of lung cancer, and proceeded to see eight more in a period of just six months.61 As a result, Dr. Ochsner and Michael E. DeBakey, MD, FACS, published "Primary Pulmonary Malignancy"62 in Surgery, Gynecology & Obstetrics (which would later be renamed the Journal of the American College of Surgeons), marking the first time tobacco use was linked to lung cancer.63 Dr. Ochsner strongly believed that cigarette smoking was the principal cause of the growing epidemic of lung cancer, and he espoused this theory in the face of ridicule and attacks, even from within the medical profession. His standard reply to critics among his peers: "Only two kinds of physicians do not accept the evidence of a causal relationship between cigarette smoking and cancer: employees of the tobacco industry and some addicted to cigarette smoking." The Ochsner Clinic, which he cofounded in 1942, eventually evolved into the Ochsner Health System. Today the institution recognizes outstanding scientific achievements that have provided pivotal insights into the fundamental biological and clinical mechanisms that relate tobacco consumption to human disease by awarding the Alton Ochsner Award Relating Smoking and Disease.64
Citations



