
The ATLS® course and the trauma center verification program set the standards for care of injured patients. Laparoscopic cholecystectomy marked a major advance in minimally invasive surgery. Surgical firsts: fetal surgery and a robot-assisted operation.
1980
Plane Crash Spurs Advanced Trauma Life Support (ATLS®) Course
1980
Plane Crash Spurs Advanced Trauma Life Support (ATLS®) Course
The College's Committee on Trauma (COT) launched its inaugural Advanced Trauma Life Support (ATLS®) course to address management of the trauma patient immediately upon arrival at a hospital.149 Based on the premise that the greatest threat to life should be treated first, the goal of ATLS is to teach a simplified and standardized approach to caring for trauma patients. The idea for ATLS got its start in 1978 after the tragic crash of a private airplane piloted by James K. Styner, MD, FACS, killed his wife and injured his children.150,151 "When I can provide better care in the field with limited resources than my children and I received at the primary facility, there is something wrong with the system, and the system has to be changed … simply put, you have to train them before you can blame them," Dr. Styner said.152 A trial course was given to a small group of Nebraska physicians, and when news of the "Nebraska course" spread, the College began to train instructors and conduct its own courses in 1980. More than one million physicians in 60 countries have taken the ATLS course, which is now widely accepted as the standard of care for initial assessment and treatment in trauma centers.153
Citations

1981
First Open Fetal Operation Performed
1981
First Open Fetal Operation Performed



Michael R. Harrison, MD, FACS, and colleagues at the University of California, San Francisco, performed the first open fetal operation. Dr. Harrison and his team corrected a dangerously blocked urinary tract in a fetus by sewing into place a bladder shunt, a little tube about the size of dry spaghetti.154-156 Dr. Harrison said that at the time "everyone was a skeptic and that's not surprising because the idea of fetal surgery was sort of shocking."157 Although fetal intervention started with crude surgical tools used to cut and sew during open operations, it quickly evolved through minimally invasive techniques and endoscopic and image-guided manipulation.158 Dr. Harrison was the recipient of the College's 2002 Jacobson Innovation Award.159
Citations
1981
Burn Patient Saved by Artificial Skin

1981
Burn Patient Saved by Artificial Skin


For the first time, artificial skin was successfully used to treat a burn patient by John F. Burke, MD, FACS. In 1969, Dr. Burke, a Harvard University medical professor and general vascular surgeon at Massachusetts General Hospital in Boston, had made a request of Ioannis Yannas, PhD, a professor of fibers and polymers in Massachusetts Institute of Technology's department of mechanical engineering: using ordinary substances, develop a flexible material to protect against infection and dehydration that looks like normal skin and will not be rejected by a patient's immune system. Consisting of a top layer of thin plastic sheet and a bottom layer of cow tendons and shark cartilage, the artificial skin acted as a seed bed for healthy skin cells taken from the patient's body. The two men said neither could have created the product on his own since it required a command of two different spheres of knowledge: the biology of the skin and the engineering of polymers.160 The synthetic human skin, now called "Integra," would save the lives of innumerable severely burned people worldwide.161 Dr. Burke was the recipient of the College's 1999 Jacobson Innovation Award.162
Citations

1985
College Fought for GME Funding on Capitol Hill
1985
College Fought for GME Funding on Capitol Hill
Reflecting the College's desire to take a more proactive role in health policy issues, George F. Sheldon, MD, FACS, a College Regent, testified before the U.S. Senate about the dangers of restricting funding for graduate medical education (GME) as a way to save Medicare dollars. GME funding was subsequently granted for five years of surgical specialty training instead of three years as proposed in the draft budget. This five-year requirement remains intact in today's Medicare law.
1985
First Robot-Assisted Surgical Procedure Performed

1985
First Robot-Assisted Surgical Procedure Performed
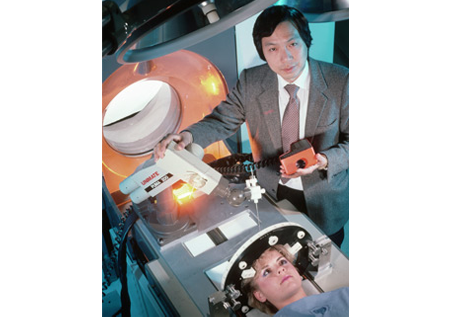
A robot named "Ole,"163 using a software interface developed by Yik San Kwoh, MD, assisted in performing a brain biopsy, in which tissue samples were removed from suspected brain tumors that would have been difficult to reach by conventional means. The novel procedure was performed at Long Beach Memorial Medical Center, Long Beach, CA, where Dr. Kwoh was director of research in the radiology department. The robotic arm's great accuracy eliminated the need for general anesthesia, reduced trauma to the brain, and allowed patients to go home the day after brain surgery instead of a week or more after.164
Citations

1987
Trauma Center Verification Program Launched
1987
Trauma Center Verification Program Launched

The College's Committee on Trauma (COT) began developing the first standards for its trauma center verification program. The program promoted the development of trauma centers that provide the hospital resources necessary to address the entire spectrum of care—from pre-hospital to rehabilitation—required for injured patients. Verified trauma centers must meet essential criteria that ensure trauma care capability and institutional performance. There are four levels—for instance, "Level I" indicates the ability to treat the most challenging and complex trauma patients. The overarching goal is to provide timely, appropriate care suited to the needs of each trauma patient. And studies show the program works: The National Study on the Costs and Outcomes of Trauma showed that patients are 25 percent more likely to survive when they receive care at a Level I trauma center than when they receive care at a non-trauma center.165 Today, there are 366 COT-verified trauma centers in the United States.
Citations
1989
Technique for Laparoscopic Procedures in General Surgery Established

1989
Technique for Laparoscopic Procedures in General Surgery Established
During the 1980s a trio of French surgeons—Prof. Philippe Mouret (Lyon), Prof. Francois Dubois (Paris), and Prof. Jacques Perrisat (Bordeaux), borrowed laparoscopic equipment from gynecologists and somewhat independently began refining an approach to perform laparoscopic general surgical
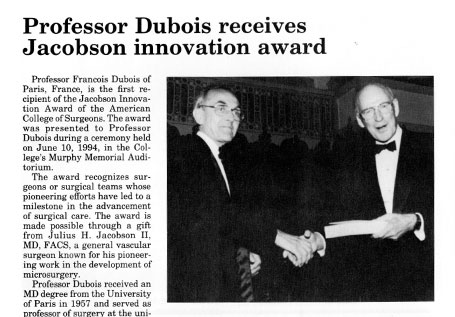
procedures—particularly cholecystectomy (surgical removal of the gall bladder).166 By autumn 1989, this "French Technique" quickly gained worldwide attention among surgeons following presentation reports of its successful use in patients by Profs. Perrisat and Dubois at surgical meetings in the United States. In January 1990, Prof. Dubois published preliminary results of the technique in 36 patients for an American medical audience in the Annals of Surgery.167 Professor Dubois would later receive the inaugural Jacobson Innovation Award of the American College of Surgeons (1994)168 for his accomplishments in this field and Professor Perrisat was named the 2011 recipient of the SAGES George Berci Lifetime Achievement Award in Endoscopic Surgery.169 Based on the initial work of these three French surgeons, a laparoscopic surgical approach is now a regular part of the general surgeon's armamentarium, and patients who are qualified candidates for the procedures are routinely offered a minimally invasive approach to selected abdominal operations, which results in less scarring and pain, and quicker recovery times.
Citations



